Intermittent catheters
Intermittent catheters are used for the technique known as 'intermittent catheterisation'. They are simple tubes with a smooth, rounded tip at the end that is passed into the bladder. On the sides of the catheter near the rounded tip there are small holes (eyelets) that allow urine to enter the catheter.
Intermittent catheters usually have a wider funnel-shaped outer end. This can be connected to a collection bag, and makes it easier to grip and direct the catheter during insertion and urine drainage.
1
Intermittent catheters in different lengthsWhat is intermittent catheterisation?
Intermittent catheterisation is used by many people to manage urinary retention. This is a condition in which the bladder fails to empty either partially or completely.
It is a procedure in which the catheter is passed into the bladder to drain urine and then is removed once drainage has stopped. This is usually done by the person themselves (intermittent clean self-catheterisation) or by a helper.
Many people successfully use intermittent catheterisation both in the short-term (for example, while waiting for an operation) and the long-term (for example, following a spinal injury). Use of intermittent catheterisation avoids the need for an indwelling catheter.
Would intermittent catheterisation be suitable for me?
Although it does not suit everyone, many people prefer intermittent catheterisation because it gives them more control and seems more “normal” than having an indwelling catheter. Whenever they need to empty their bladder, they visit the toilet to catheterise.
Intermittent catheterisation should only be done after a thorough assessment and training in the procedure by a healthcare professional.1 For some people with neurological or physical disabilities, learning to do intermittent catheterisation may take longer and require an extended learning period.
The frequency of catheterisations per day is usually a decision made jointly with a health care professional. This varies from person to person and depends upon clinical considerations such as the degree of retention experienced as well as lifestyle considerations.
Although intermittent catheters can be used by people with a wide range of physical difficulties (including impaired vision, tremor and reduced sensation), success is more likely if you have:
-
A positive attitude towards the procedure – starting intermittent catheterisation can be very daunting, but research has shown that good information, together with thorough teaching and good communication with your health care professional, can help you to adapt to intermittent catheterisation successfully both when you are new to it and in the long-term.
-
Reasonably good hand control – opening packaging, lubrication and inserting the catheter can be difficult for some people, although there are some products that can help.
-
A good memory as regular catheterisation at the correct time is important. You must catheterise according to the regime agreed between you and your health care professional. This may be a few times a week or several times a day. It is important that you do not forget. If your bladder becomes overfull, you may experience bladder leakage and, in the long-term, this build-up of urine can cause damage to your kidneys.
Some people are unable to self-catheterise, in which case a helper such as a family member can be taught to do it.
Although the catheter is usually passed through the urethra, other catheterisable channels such as a mitrofanoff diversion or cystostomy button can be used.
| More likely to suit you if... |
Less likely to suit you if... |
- You have a residual urine volume of more than 100ml
|
- You do not feel motivated to use the technique
|
- You (or your helper) find the idea of clean intermittent catheterisation acceptable
|
- Alternative non-invasive methods of managing your bladder are available
|
- Your hand control is good enough to manage intermittent catheterisation or you have a helper
|
|
- Your memory and mental capacity are good enough to manage intermittent catheterisation or you have a helper
|
|
How are intermittent catheters used?
Most intermittent catheters are provided in waterproof, airtight packets. After removal from the packet, some may require a lubricating or anaesthetic gel to be applied before use, while others have their own built-in, water-activated lubricant.
The catheter is passed gently through the urethra and into the bladder until urine starts to flow. The stream of urine can be directed straight into a toilet or, if there is no accessible toilet, a suitable container. An alternative is to attach the funnel end of the catheter to a urine collection bag or use a catheter with an integral collection bag
Selecting intermittent catheters
There are many brands of intermittent catheter available, incorporating different features (for example, catheter material, coatings, collection bags) designed to make intermittent catheterisation easier depending on your circumstances.
Intermittent catheters come in three main types:
-
Non-coated catheters These are the traditional intermittent catheter design. To make insertion easier, non-coated catheters can be coated in a lubricant jelly or a local anaesthetic gel before use. This is particularly important for men. Women may choose to use them either with or without a lubricant or dip them in water for slight lubrication.2
-
Coated catheters These catheters have a “hydrophilic” coating that forms a slippery lubricant layer when the catheter is soaked in water (usually for around 30 seconds) before use. Many people soak the catheters by filling their packaging with water.
-
Pre-lubricated catheters These catheters are supplied pre-packed with a coating of water-soluble gel. They can be used straight from the packet with no additional preparation.
Despite a considerable number of trials, there is no evidence to suggest that any of the basic intermittent catheter types are better than any other for most users.3
Therefore, deciding which type to use is a matter largely for personal preference (including comfort and cost) and availability.
Your choice of catheter may be influenced by the material from which they are made. Most intermittent catheters are made from polyvinyl chloride (PVC), a commonly used plastic, although catheters are also available in other materials. They are stiff enough to make insertion easier, but pliable enough to pass through the bends in the male urethra. The female urethra is relatively short and straight, and therefore easier to pass a catheter through. Some brands are softer than others e.g. silicone catheters, and you may need to try different brands to find the one that suits you best.
Do intermittent catheters come in different sizes?
Intermittent catheters are available in different lengths and sizes to suit men and women.
Catheter length
-
Male length catheters (up to 40cm) - men have a relatively long urethra and therefore need a male length catheter.
-
Female length catheters (up to 20cm) – women have a much shorter urethra and therefore can use the shorter, female length catheters. Some larger women or those with reduced mobility sometimes prefer to use a male-length catheter.
-
Female Compact catheters (length 7cm) - female compact-size catheters are available, they have been found to be as effective as longer 20cm length catheters and are discreet for carrying.4
-
Male compact catheters are available, but it is the packaging that is compact rather than the catheter, as men will almost always require a longer length catheter.
5
Discreet intermittent catheters for men and womenCatheter size
Catheter size relates to the thickness or external diameter of the catheter and is measured in French Gauge (FG or FR) or Charrière (Ch). A Ch equals 1/3 of a millimetre - so a 12Ch catheter is 4 millimetres in external diameter.
Most catheters range in size from 10Ch to 20Ch. Size 10Ch or 12Ch is usually suitable for women. Sizes 12Ch, 14Ch or 16Ch is usually suitable for men. Smaller sizes are available for use in paediatrics (e.g. 8Ch).
It is recommended that you use the smallest size to maintain good drainage and reduce the risk of urethral and bladder neck trauma.5
Products that can make intermittent catheterisation easier
Some catheter manufacturers produce items that are intended to make using or carrying catheters easier and more discreet.
For example, conveniently packaged ‘catheter-sets’. These can include separate or integrated pouches of water for use in soaking coated catheters or an integrated urine containment pouch inside the pack. These products can be useful if you are catheterising with poor or no access to clean water and/or toilet facilities.
3
Foldable intermittent catheter for easy carrying8
Intermittent catheter with non-touch introducer You may prefer to use a mixture of catheter types, depending on your personal circumstances and lifestyle.6 For example, using catheter sets - which tend to be more expensive - on holiday, and standard catheters when at home or near a toilet.
If you have difficulty with your hands or mobility, there are several devices available that may make it easier for you to do intermittent catheterisation - see Catheter accessories.
Is intermittent catheterisation a sterile procedure?
Intermittent catheterisation can either be a sterile or a clean procedure:
-
Sterile procedure - this is necessary in hospital or a care home, or if the catheterisation is being done by a healthcare professional who has contact with several patients.
-
Clean procedure - people doing self-catheterisation generally follow a clean procedure. A clean procedure may also be used for catheterisation by a helper who only looks after only you e.g. a family member (clean intermittent catheterisation). A ‘clean procedure’ simply means that you wash your hands and follow usual basic hygiene procedures before, during and after catheterisation.
Can intermittent catheters be reused?
Policy and practice vary around the world with regards to the reuse of intermittent catheters.7 In some countries single-use catheters are the norm, while in many other countries the reuse of catheters, even those licensed for single use, is commonplace.8 Currently there is no convincing evidence that single-use catheters prevent urinary tract infections, urethral trauma or haematuria.3910
28
Reusable silicone intermittent catheter with cleaning/storage tubeAlthough coated catheters should be used only once and then thrown away, around the world many people re-use uncoated PVC or silicone intermittent catheters, washing them after each use and storing them in a clean receptacle. Cornstarch catheters are now available that can be cleaned and re-used for 24 hours.
The decision to use single-use catheters or to reuse non-coated catheters depends on many factors. In some health systems, single-use catheters are supplied to users free of charge, whereas in others, catheters are an out-of-pocket expense, so that re-using them saves money in terms of catheters purchased. Some people report improved quality of life using “ready-to-use” single-use catheters.7 However, others feel that reusing catheters may be more discreet (avoiding the need to carry and dispose of multiple single-use catheters and packaging) or prefer reuse due to concerns about environmental issues (most catheters are not bio-degradable and contribute to landfill).8
You may find that 'mixed use' using a combination of single-use and re-usable catheters works best for you. For example, re-using your catheters when at home and using single-use disposable catheters at times when you can’t easily wash the catheter after use.
How do I dispose of single-use catheters?
If possible, rinse the catheter through and wrap in the catheter packaging or a plastic bag. Catheters may be disposed of in the household waste.
How much do intermittent catheters cost and where can I get them?
The cost of intermittent catheters varies according to the brand and which country you live in.
-
In the UK, most catheters are available on prescription from a family doctor. If you do not have to pay prescription charges, this will mean the catheters are free to you. Alternatively, catheters can be obtained free of charge from agencies on behalf of the catheter manufacturer, who are then reimbursed by the NHS.
-
In some other countries such as the US, depending on your insurance programme, it may be possible to get reimbursement for your catheter costs. Speak to a healthcare professional for local advice in your country.
-
If you use a new catheter every time, then the cost for the catheters will be higher than if you clean and reuse them.
-
Specialist continence health care professionals may be able to provide you with some samples from different manufacturers. Alternatively, look on manufacturers’ websites. Many offer free samples/trial packs. This can be a good way to try out the different types and find out what will work for you.
Click here to find organisations where you live for local information about availability, access and cost.
Difficulties with intermittent catheters: What do I do if…
I am having difficulty gripping the catheter?
Try using catheters where the coating (and therefore the slippery surface) ends a few centimetres from the funnel end. This means there is an easier to grip section.
Some catheters and manufacturers provide handles to help with gripping the catheter during insertion and there are aids available to help you - see Catheter accessories.
I am having difficulty finding the urethral opening?
Women can find it particularly difficult to identify the urethral opening. This is especially true for women with mobility difficulties. With practice, some women are able to do this by touch, others require a mirror. Leg spreaders are available to help with parting your legs and keeping them apart throughout catheterisation. Some of these also have a mirror and / or light attached to help see the urethral opening - see Catheter accessories. Experiment with the best position for catheterising – this may be on the toilet, in your wheelchair or possibly on the bed or even a firm surface such as the floor.
I am having difficulty inserting the catheter?
Some men find it difficult to stretch out the penis into a position for catheter insertion. A penis holder can help to support the penis in a good position while you insert the catheter - see Catheter accessories.
If you find the catheter bends very easily during insertion, you could try a more rigid, plastic catheter or one with a soft, curved, coude tip.
I experience bleeding when I remove my catheter?
Slight bleeding is not uncommon with intermittent catheterisation. You need to think about the catheter lubrication. If you are using an uncoated catheter, use lots of lubricant, particularly if you are a man. Alternatively, you may wish to try a hydrophilic catheter if bleeding is an on-going problem.
You should contact your health care professional if bleeding is more than slight or persists.
The catheter is sticking when I insert or remove it?
If you are using an uncoated catheter you may want to try using more lubricant or try a coated or pre-lubricated catheter.
If you are already using a coated catheter you may wish to try another brand, to see if that works better for you. Ensure that you are soaking the catheter for the correct amount of time before use.
If it sticks on removal, you may be leaving the catheter in your bladder for too long. Ensure you remove the catheter as soon as urine has stopped draining. If it is taking a long time to drain the urine, you may need to consider using a larger sized catheter for speedier drainage.
I am having repeated urinary tract infections?
If you are getting repeated infections, it may help to think about your technique.
Common reasons include:
-
Inadequate hand-washing - check that you are thoroughly washing and drying your hands. The fingertips, palm of your hand and thumb are commonly missed areas.
-
Cleaning method for reused catheters – if you are reusing your catheters, make sure you are cleaning your catheter thoroughly after each catheterisation. Cleaning non-coated catheters using soap and water and a 15-minute soak in Milton fluid has been shown to leave them free of the organisms that can cause infection. 1112 At present there is no good evidence to show that cleaning and re-using uncoated catheters is more likely to cause urinary tract infection than single-use catheters.3910
-
Incomplete drainage – it can be frustrating while in the toilet waiting for your catheter to drain. However, it is important that you allow the urine to drain completely. If it is taking an unacceptably long time, try using a larger size catheter. Always discuss any increase in catheter size with a health care professional.
I am having difficulty accepting that I must do intermittent catheterisation?
Catheterisation is an invasive procedure and understandably some people dislike it and choose not to do it. Good information together with thorough teaching and good communication with your health care professional can help you to adapt to intermittent catheterisation successfully both when you are new to it and in the long-term.13
However, some people really find intermittent catheterisation too difficult. If you have explored all options for intermittent catheterisation and tried different products to help overcome your difficulties, then you should discuss alternatives with your health care professionals – for example, catheterisation by a helper or an indwelling catheter.
Where can I get intermittent catheters?
The cost of catheters varies according to the type and which country you live in. If you live in the UK, then you will be able to get your catheters prescribed from the family doctor. In some other countries such as the US, depending on your insurance programme, it may be possible to get reimbursement for your catheter costs. Speak to a healthcare professional for local advice in your country.
Indwelling catheters
Indwelling catheters (also called Foley catheters) are designed to remain in the bladder continuously for a period of time.
The inner end (tip) of the catheter simply sits in the bladder where it is held in place by a small balloon that is inflated with sterile water after the catheter has been inserted.
Small holes (eyelets) at the catheter tip allow urine to drain freely from the bladder through the tube. The outer, funnel end of the catheter is usually connected to a collection bag, where urine is stored prior to emptying. Alternatively, the catheter may be connected to a catheter valve which is opened as needed to allow intermittent emptying of the bladder.
Apart from new materials and changes in small details, the design of indwelling catheters has remained the same for decades. Research is ongoing to improve performance and safety, including a new balloon shape, changes in tubing design to optimise flow, and additional eyeholes.141516
Indwelling catheters can be hazardous if used incorrectly. Read the guidance below for important safety information.
Additional information is available for Men managing a catheter after prostate surgery.
Discover more information and hear people talking about the experience of living with a catheter.
10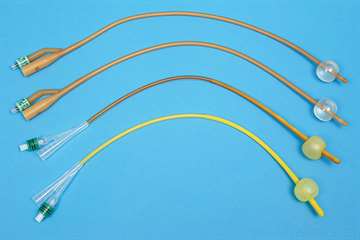
Selection of Foley indwelling catheters
| More likely to suit you if... |
Less likely to suit you if... |
- Your leakage is associated with urinary retention
|
|
- You (or a helper) are unable to do clean intermittent catheterisation
|
- You have poor memory and mental function
|
- You have found pads to be unsuccessful or inappropriate
|
- Urinary tract infection is a major concern for you
|
- Your skin is severely damaged in the pad area
|
|
Categories of indwelling catheters
There are two types categorised according to their route of entry into the body:
-
Urethral catheters are the most common type of catheter. They are inserted into the bladder via the urethra, the narrow passage through which urine normally passes from the bladder.
-
Supra-pubic catheters are inserted into the bladder via a small cut through the abdomen above the pubic bone (during a small surgical procedure). They are typically used for long-term bladder management but may in some instances be used in the shorter term after certain types of surgery.
The same types and makes of catheters are used for both urethral and supra-pubic catheterisation, although not all urethral catheters are licensed for supra-pubic use.
Indwelling catheters can also be classified according to the length of time that the catheter is in place:
The material that the catheter is made from differs according to whether it is a short or long-term catheter.
Who are indwelling catheters good for?
Indwelling catheters are useful for people who are unable to empty their bladder normally and for whom intermittent catheterisation is not an option.
Common circumstances in which an indwelling catheter may be used include:
-
Acute urinary retention or ‘bladder outlet obstruction' when waiting for, or unsuitable for, medical or surgical treatment.
-
Chronic urinary retention if intermittent catheterisation is not feasible.
-
Immobility or incapacity if it is the only viable option for managing the bladder in the longer term for debilitated, paralysed or comatose people.
-
Following surgery to allow for healing (for example, after prostate surgery to allow the urethra to heal) or because there is a risk of post-operative urinary retention. Depending on the type of surgery, in most cases the catheter will only be in place for a few days or weeks.
-
Pressure ulcers or non-healing incontinence associated dermatitis to allow healing by preventing contamination of the skin by urine.
-
Intractable urinary incontinence when a catheter can improve quality of life and other non-invasive options have been considered.
An indwelling catheter should only be used after a detailed assessment of your needs has been made by a health professional who has discussed the implications of having a catheter with you. You should know why it has been recommended and the planned length of time for it to remain in place.
Because of the high risk of complications from indwelling catheters such as urinary tract infection, an indwelling catheter should only be considered when all the other product options have been fully explored.
Frequently asked questions about indwelling catheters
What is the difference between male and female catheters?
-
Catheters for men are longer than those for females - men have a much longer urethra than women. Male catheters are usually up to 40cm long. Female catheters are usually up to 20cm long.
-
Some women, particularly those who are larger or less mobile, prefer to use a male length catheter, as they can access the outer funnel end of the catheter more easily. Supra-pubic catheter users may also prefer the longer length catheter.
-
Men should not use female length catheters as the shorter length risks inflation of the retention balloon inside the urethra rather than the bladder. When inserting a catheter in men, it is recommended to insert it to the bifurcation (this is the part furthest from the body where the catheter divides into two channels - one for the urine drainage port and one for the balloon port).17 This helps to ensure that the catheter tip is in the bladder before the balloon is inflated.
What do the different catheter sizes mean?
Catheters are traditionally measured using Charriere (Ch) or French gauge (FG or FR). The measurement relates to the external diameter of a catheter. The Ch is 3 times the size in millimetres (mm). For example, a Ch12 would be 4mm in diameter. However, the internal diameter of the tube varies according to the manufacturing process and is narrower in coated catheters.
-
Urethral catheters are most frequently used in sizes 10-12Ch for women and 12-14Ch for men.
-
The most commonly used size for an adult supra-pubic catheter users is 12-16Ch.
-
The funnel end will usually have the catheter and balloon size printed on it.
Your healthcare professional should advise you on the best catheter size. The smallest size to maintain good drainage and prevent urethral and bladder neck trauma should be used.5
The largest size used in routine indwelling catheterisation is usually 16Ch. However, it may be necessary for medical reasons, such as passing blood clots after surgery or debris in the bladder, to use larger catheter sizes and catheters are available up to size 26Ch/Fr.
Why do indwelling catheters have a balloon?
The inside end of the catheter simply sits in your bladder and is not attached in any way. To prevent the catheter from slipping out, the small balloon near the inside end of the catheter is inflated with sterile water.
Standard (two-way) catheters, have two separate channels: one is for urine drainage and the other allows sterile water to be introduced to inflate the balloon.
Some specialist types of catheter have three channels (three-way catheters). The third channel enables the bladder to be continuously flushed after prostate or bladder surgery to remove blood and clots.
Which balloon size is suitable for which people?
A 10ml balloon is recommended as standard for adults. Larger sizes are available, but it is recommended that the smallest balloon size is used, where possible, to prevent bladder discomfort and irritation.
Larger balloons (30ml) tend to sit higher in the bladder and there is the potential for urine to collect below the catheter eyelets, preventing the bladder from draining fully. They are also associated with increased risk of bladder spasms, which may cause the catheter to be forced out with the balloon still inflated and cause damage to the delicate tissue of the urethra and the bladder neck.
It is important that the balloon is inflated with the correct amount of sterile water, so the balloon sits comfortably just inside the bladder.
There is some evidence that using sterile water to inflate the balloon in silicone catheters can lead to gradual water loss from the balloon.18 This could lead to the catheter falling out.19 Some manufacturers recommend either filling the balloon with a 10% aqueous glycerine solution or filling the balloon with the full 10ml and being aware that ¼ to ½ could be lost over time.18
Are there any disadvantages to using indwelling catheters?
Indwelling catheters are rarely trouble-free and should only be used as a final option, when all other product and treatment options have been explored.
If an indwelling catheter is necessary, the need for it should be reviewed at regular intervals and it should be removed promptly if it is no longer necessary.
What problems might I experience if I have a short-term catheter?
Short-term indwelling catheters are usually used during episodes of acute ill health often in hospital e.g. after an operation and/or for accurate measurement of urine output. The major problem associated with their use in this situation is a hospital-acquired catheter-associated urinary tract infection. This can have serious consequences for people who, through ill health, are particularly vulnerable to infection and may also contribute to the development of antibiotic-resistant microorganisms.12021
What problems might I experience if I have a long-term-term catheter?
For some people, a long-term catheter can provide satisfactory management of bladder problems and greater independence. However, they are associated with several problems:
-
Increased risk of infection - long-term indwelling catheters can lead to catheter-associated urinary tract infections.
-
Recurrent blockage - due to encrustation by mineral deposits following infection with certain types of bacteria.
-
Damage to the delicate tissue near the urethral opening - often caused by excessive weight from heavy urine drainage bags pulling down on the catheter.
-
Bladder spasms – the bladder’s response to a foreign body in it; these can sometimes be strong enough to force the catheter out of the bladder with the balloon inflated.
-
Bladder stones – there is an increased risk of bladder stones forming in users with spinal cord injury compared to those using intermittent catheterisation.2223
-
Pain and discomfort - which can be distressing.
-
Negative impact on body image - and effect on sexuality.
If intermittent catheterisation is possible, it should be considered. It is less invasive, is generally associated with fewer risks and can allow a greater degree of independence.
If a catheter is expected to be in place long-term (i.e. >14 days), the catheter should be made of a material designed for long-term use (all-silicone, silicone or hydrogel-coating).
How often should a long-term indwelling catheter be changed?
There is no good research evidence to tell us how often a long-term indwelling catheter (either urethral or suprapubic) should be changed.24 They are intended to remain in place for up to 12 weeks but, in practice, this varies. Some people are more prone to catheter blockage than others and may need their catheter changed more frequently.2526
What should I do if I have blood in my urine?
A small amount of blood in your urine is common just after the catheter has been inserted. At other times it could be a sign of an infection.
If the bleeding is heavy, or you see clots in your urine, especially if your catheter isn’t draining properly, you should seek advice from a healthcare professional.
How should I clean my catheter?
Indwelling catheters are single-use items and are thrown away after removal. While in place, you should clean round the catheter carefully with soap and water at the point where it enters the urethra, to ensure good personal hygiene.2728 It is not necessary to use antimicrobial solutions, although use of a mild chlorhexidine solution for meatal cleansing prior to catheter placement and during routine cleaning may reduce infections.20293031
Supra-pubic catheters are often covered with a dressing at the insertion point, although once the insertion site has healed some people choose not to use a dressing. The skin around the supra-pubic site can be cleaned with sterile water (or cooled boiled water) or saline (salt water). If you notice a discharge from the entry point or it becomes red and inflamed, you should ask a health professional for advice.
Difficulties with indwelling catheters: What do I do if…
I am having frequent urinary tract infections?
Most people with an indwelling catheter for more than a few days will have bacteria in the urinary tract (bacteriuria). However, this does not always mean that they are considered to have a urinary tract infection that needs to be treated. There are two types:
-
Asymptomatic bacteriuria – This means bacteria can be detected in the urine, but the person feels well and has no symptoms of urinary tract infection. Asymptomatic bacteriuria should not generally be treated with antibiotics.
-
Symptomatic bacteriuria – This means bacteria can be detected in the urine and the person has sudden symptoms of urinary tract infection such as high temperature (fever), pain over the lower abdomen or loin (mid-back) pain, dizziness or confusion, offensive smelling urine, or pus/blood in the urine. If you have a spinal cord injury you may also need to look out for increasing spasticity and / or worsening autonomic dysreflexia (usually shown by an increase in blood pressure, headache, sweating above the SCI lesion, flushing below the SCI lesion) or a “sense of unease”. Symptomatic bacteriuria requires treatment with antibiotics and you should contact your health care professional.
Bacteria can attach themselves to the catheter causing a 'biofilm'. In this state, antibiotics may be ineffective. Therefore, in preparation for and during antibiotic treatment, your health care professional may also recommend the following:
-
Replacement of the indwelling catheter with a new catheter - there is some research evidence that this might be beneficial immediately before starting antibiotics.32
-
Removal of the indwelling catheter and use of intermittent catheterisation (if you or a helper is able to do it).
-
Removal of the indwelling catheter and use of pads.
Some things may help to reduce the risk of repeated symptomatic urinary tract infections:
-
Simple good personal hygiene can be important in reducing the risk of urinary tract infections. For example, cleaning around the area where your catheter exits your urethra with soap and water.2728 It is not necessary to use antimicrobial solutions, although recent research has found that in men meatal cleansing with a mild chlorhexidine solution prior to catheter placement can reduce subsequent infections, and that use of mild antimicrobial solutions during routine cleaning while a catheter is in place may also reduce infections.20293031
-
Maintaining a closed drainage system - it is important that the connection between the catheter and the drainage bag or catheter valve is not disrupted unnecessarily, as this is a route through which bacteria can access the urinary tract. If you use a large capacity urine collection bag when in bed, this should be connected to the body-worn bag via the drainage tap, rather than disconnecting one bag and connecting the other - this is called a 'link system'. The emptying tap on the body-worn bag should be left open to allow urine to flow through it and into the larger one.
Some things are commonly thought to reduce the risk of repeated symptomatic urinary tract infections, but in fact there is no evidence that they are helpful:
-
Regular routine urine culture - taking a sample of urine and analysing it is not necessary in catheter users who are otherwise well.
-
Prophylactic antibiotics - the routine use of antibiotics or using antibiotics before a catheter change is not recommended in preventing infection in long-term catheter users.33 This practice can lead to the development of bacteria which are resistant to antibiotics.
-
Disinfectants - adding disinfectants to drainage bags and bladder irrigation is not recommended.34 There is no evidence that this is effective as a routine infection-control measure.
-
Cranberry juice - drinking cranberry juice has been shown to be beneficial for some people with frequent urinary tract infections, but it has not been shown to benefit catheter users specifically.35
-
Type of catheter – although efforts have been made to develop catheters that prevent urinary tract infections, none have yet been successful for long-term use. Different catheter coatings, such as silver alloy, have not been found to reduce the risk of urinary tract infections in short-term use.363738
My catheter keeps blocking?
Catheter blockage is very common. In short-term catheters after surgery, this can be due to blood clots blocking the eyes of the catheter. Some specialist types of catheters have three channels inside (three-way catheters). The third channel enables the bladder to be continuously flushed, for example, after prostate or bladder surgery, to remove blood and clots.
In long-term catheters, blockage is usually due to encrustation by mineral deposits around the eyelets and tip of the catheter or inside the catheter lumen (the hollow passage through which urine passes). Also, debris/stones can develop in the bladder and prevent the catheter draining freely. Recurrent urinary catheter blockage caused by encrustation occurs in 40-50% of all long-term catheterised patients
Establishing a pattern of blockage
- If your catheter becomes blocked, it is likely you will need to have it changed. If you are experiencing repeated blockages requiring catheter changes, it may be possible to establish a ‘pattern of blockage’. Make a record of how long each catheter lasts before blockage occurs and try to arrange to have your catheter changed before blockage occurs. For example, if your catheter only lasts 6 weeks before blocking, arrange with your healthcare professional to change it every 4 weeks.
Trying different materials
-
Although catheters are currently available in various materials and tip designs, none are completely resistant to encrustation, although the time taken for blockage to occur varies between the different catheter materials.3940
-
There is some evidence that catheters with a narrower lumen (the hollow inside of the tube through which urine passes) block more quickly than those with a wider lumen.3940 Catheters made from 100% silicone are uncoated and therefore have a slightly wider lumen than other, coated types, so may be worth trying. But they do tend to be stiffer than other types of catheters and some people can find this uncomfortable.
Bladder washouts
-
Catheter “washout solutions” are available that are intended to reduce encrustation. However, there is no clinical evidence that they are effective.7
-
None of the currently available solutions will completely prevent catheter blockage, but they may extend the time a catheter can be left in place.41
-
There is some weak research evidence that citric fruit juices (orange, lemon and lime juices) and water intake may be helpful by changing urine acidity and reducing encrustation.424344
Urine is leaking around my catheter?
Sometimes urine can leak from around a catheter, rather than draining through it. This can occur if:
-
Drainage of urine through the catheter is prevented either by a blocked catheter (see above) or if the drainage bag tubing is accidentally compressed or kinked.
-
Bladder spasms occur – the presence of the catheter in the bladder and/or a build-up of urine in the bladder can cause the bladder to contract strongly, resulting in urine being squeezed out around the catheter. If this happens repeatedly, talk to your healthcare professional. They may recommend taking medication to reduce bladder contractions.
-
Check that you are using a standard balloon size (10ml is recommended for adults) and that it is inflated with the correct amount of water. A balloon which is over-inflated or too large (30ml) may irritate the bladder leading to spasm. Also, if you have too large a balloon, it might be sitting too high in the bladder and not draining the bladder completely.
My catheter is dragging/pulling down?
-
A drainage bag that is heavy with urine can pull down on the catheter. This can cause discomfort, movement of the catheter and, if allowed to continue, damage to the urethra and bladder neck.
-
If using a leg bag, try different ways of holding it in place using combinations of straps in different positions, net support garments and suspension belts.
-
Consider using a smaller leg bag and/or emptying it more frequently. A bag holding 500ml will weigh at least 500g, which can be quite a lot to support on your leg. Leg bags are available with as little as 250ml capacity.
-
Special drainage bags that are worn around the abdomen and supported with waist straps are also available.
-
Supporting the catheter tubing on your leg and preventing it from moving too much can also help reduce dragging on the catheter. You could consider a stabilisation device, which attaches to the leg using adhesive to hold the catheter firmly in place. As well as reducing tugging, there is some research evidence to suggest that this prevents the ‘to and fro’ movement of the catheter that allows bacteria to enter the bladder.45
-
If you have good use of your hands and can remember to open the valve and empty your bladder regularly throughout the day, then using a catheter valve instead of a leg bag during the day be suitable.
How much do indwelling urethral catheters cost and where can I buy them?
The cost of catheters varies according to the type and which country you live in. If you live in the UK, then you will be able to get your catheters prescribed from the family doctor. In some other countries such as the US, depending on your insurance programme, it may be possible to get reimbursement for your catheter costs. Speak to a healthcare professional for local advice in your country.
Catheter accessories
There are various accessories that can be used to assist with either indwelling catheter use or the process of Intermittent catheterisation:
Catheter valves
A catheter valve is a compact device that is connected to a catheter outlet (funnel end) in place of a urine collection bag. The valve is used to control the flow of urine. When the valve is closed, it prevents urine from leaving the bladder. The valve is opened periodically to allow urine to drain from the bladder and closed once the flow stops.
Using a catheter valve means that urine is stored in the bladder and is drained by the user at regular periods throughout the day. Some people find this more normal and appreciate the freedom from wearing a urine collection bag.
The use of valves does not increase the risk of infections and may be associated with improved bladder tone and capacity and there is some research evidence to suggest that they may help reduce catheter encrustation and blockage by promoting a more natural flushing action of the bladder.2846 It is usually recommended that the valve is worn day and night for up to seven days.
Most catheter valves are designed so that they can be attached to a urine collection bag when the user is asleep, with the valve left open so that the bladder can drain freely. This means a collection bag can be used during sleep periods without removing the valve and helps to minimise the risk of micro-organisms getting into the catheter and bladder.
23
Automatic closing catheter valve22
Flip-flo style catheter valveWho are catheter valves good for?
Catheter valves are useful for people using an indwelling urethral or suprapubic catheter who have sufficient use of their hands to operate the valve and who will reliably remember to empty their bladder at regular intervals to avoid bladder overfilling.
They are generally not suitable for people who have poor use of their hands, poor bladder capacity, detrusor overactivity, ureteric reflux, renal impairment, or poor memory.
You need a full and thorough assessment by an appropriately trained healthcare professional to assess whether a catheter valve would be suitable for you.47
What other products could ‘mix and match’ well with a catheter valve?
Catheter valves can be a useful way to control urine flow from an indwelling catheter during the day, but at night or during periods of sleep, they should be connected in the open position to a urine collection bag.
Catheter valves are also used by some men who use sheath urine collection systems, and whose leakage is very light or during specific activities (such as swimming). The sheath can contain small amounts of urine leakage until the valve is opened.
Selecting catheter valves
Many designs are available. Some are more discreet under clothes than others, and some are easier to open than others.
Think about your personal priorities; for example, a larger tap or opening mechanism could be easier to open but may be less discreet under clothing. It is worth looking at all the designs available to find one most suited to your lifestyle.
It may be worth trying a few different designs to see which one works best for you. Manufacturers often offer free samples on their websites.
You can hear more about catheter valves here.
Stabilisation devices
Catheter stabilisation devices are used to prevent an indwelling catheter being tugged or pulled down by the weight of a urine bag, body movement or clothing.
This type of device can help reduce discomfort and may also reduce the risk of catheter associated infection, as they minimise the 'to and fro' movement which can allow bacteria to enter the bladder.45
Elasticated tubing support straps can be worn around the upper thigh (or abdomen for a supra-pubic catheter) to hold the catheter firmly in place; these straps may be washed and reused.
Alternatively, disposable, adhesive devices are available that may be worn for up to seven days. They stick to the leg (or abdomen for supra-pubic catheters) and are worn day and night.
If you are having problems with your urethral catheter pulling or dragging down, you can read more here about straps and support garments that are designed to support body-worn collection bags in place on the thigh or calf.
24
Adhesive multi-directional tubing support26
Tubing support leg strapIntermittent catheterisation aids
Some people find intermittent catheterisation difficult to perform for several reasons, including poor hand control. There are several devices available that may help:
Handles – intermittent catheters are small and thin and if you have a problem with your hands or find a pincer grip difficult, you might find the catheter hard to use. Special intermittent catheters are available that come with a handle already attached, or specially designed grips are available that attach to the end of the catheter (these are larger and make holding the catheter easier).
17
Handle to help with intermittent catheter insertionMirrors Women often find it difficult to locate the urethral opening. If this is the case for you, you may need a mirror / light source at least when you are learning. A self-standing mirror and angle-poise lamp can give you the visibility you need, while keeping two hands free to manage the catheter.
21
Self-catheterisation mirrorsLeg spreader - this inflatable device has a mirror attached and is designed to help separate the legs and hold them apart during catheterisation.
20
Inflatable leg divider with mirror attached for ease of intermittent self-catheterisationPenis holder – this can be used to hold and support the penis in a good position to make catheterisation easier. They are particularly useful if you have a small or retracted penis (common after prostate surgery) or if you have poor use of your hands or only have use of one hand.
16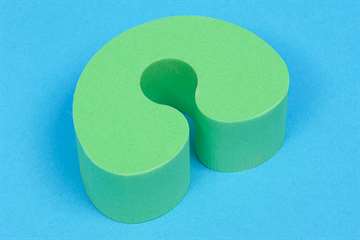
Cuff to support penis during intermittent self-catheterisationWhere can I get catheter accessories?
The cost of these products varies according to the type and which country you live in. If you live in the UK, then you will be able to get some of them prescribed from the family doctor. In some other countries such as the US, depending on your insurance programme, it may be possible to get reimbursement for your catheter-related costs. Speak to a healthcare professional for local advice in your country.